A patient with either type of peroxisomal disorder (peroxisomal biogenesis disorder or single enzyme protein deficiency disorders) can be diagnosed through several biochemical tests or by sequencing the patient’s DNA to identify which mutations a patient has.
While peroxisomal disorders affect each patient differently, common health issues include: hearing and vision loss, hypotonia, neurological issues, seizures, developmental delay, feeding issues, adrenal insufficiency, leukodystrophy, and liver, kidney, and bone disease.
In the past, there was limited early detection of peroxisomal disorders.
Now, there are two ways that individuals are being diagnosed with peroxisomal disorders. The first is what we’ll call the, “Turn over every stone” approach, and the second method is through comprehensive newborn screening shortly after birth.
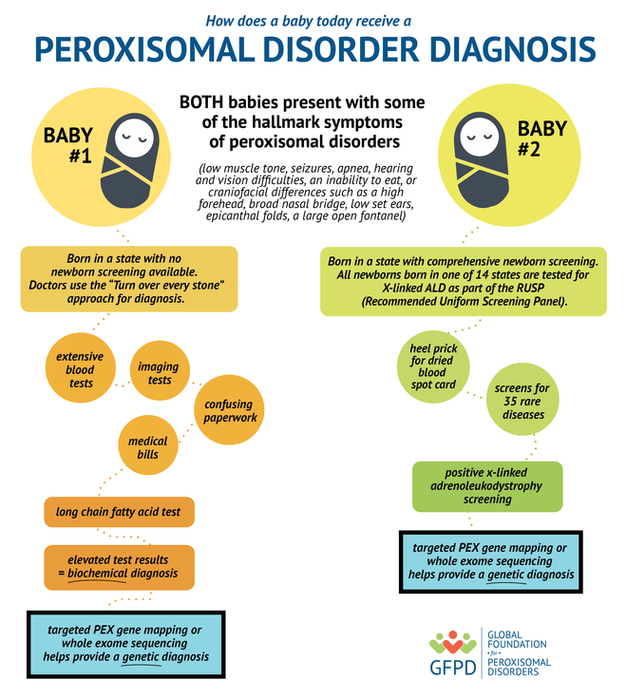
“The Turn over every stone” approach is similar to looking for a needle in a haystack. When a baby is born with some of the hallmark symptoms of peroxisomal disorders, (low muscle tone, seizures, apnea, hearing and vision difficulties, an inability to eat, or craniofacial differences such as a high forehead, broad nasal bridge, low set ears, epicanthal folds, a large open fontanel) this can kick off a series of tests run at the hospital or sometimes run after a baby is discharged from the hospital by a pediatrician or geneticist.
Many rare or congenital diseases have similar symptoms, and so usually a physician tests for a variety of rare diseases. This testing and turning over every stone can be an arduous and lengthy journey and can leave families feeling powerless and weary. While a physician is “turning over every stone” families may have to endure extensive blood tests, imaging tests, and a slew of confusing paperwork. With the “Turn over every stone approach” physicians may eventually run tests to look at the levels of very long chain fatty acids. Elevated levels of very long chain fatty acids would help provide a biochemical diagnosis of a peroxisomal disorder while targeted PEX gene mapping or whole exome sequencing helps provide a genetic diagnosis.
Early diagnosis of a peroxisomal disorder can help provide treatment options for families to discuss with their local physicians who likely have never seen this type of genetic disorder. Peroxisomal disorders affect an estimated 1 in 50,000 live births, although with earlier and expanded access to newborn screening, this number could increase in frequency.
The second (and newer) method for diagnosing a peroxisomal disorder is through comprehensive newborn screening of 35 rare diseases at birth, before the baby leaves the hospital. The Department of Health and Human Services provides guidance for states on specific diseases that all newborns should be tested for on the Recommended Uniform Screening Panel (RUSP). There are 35 such diseases that are on the RUSP, and x-linked adrenoleukodystrophy is one of them- this is the screening which also captures infants with a peroxisomal biogenesis disorder or one of the related single enzyme deficiencies. As of early 2020, 14 states have begun screening for anomalies in very long chain fatty acids, which is a marker for x-linked adrenoleukodystrophy. This newborn screening is done on ALL babies born, not just those having difficulty at birth.
States that do comprehensive newborn screening, prick the baby’s heel at birth and take a small sample for a dried blood spot card to be analyzed in a lab for all of the disorders on the RUSP that the particular state tests for. If the newborn screening test comes back positive for elevated levels of very long chain fatty acids, this can prompt doctors to order further genetic testing like PEX gene mapping or whole exome sequencing.
Once a family receives a genetic diagnosis, they can then look for additional resources, patient
communities to connect with and begin to move forward. While there is always uncertainty about what the future holds for individuals affected by peroxisomal disorders, with treatment guidelines and support from the GFPD, we can work together to provide the best possible resources for families, therapists, educators and medical professionals.
